Improving Access and Outcomes Using Success, Effort, Emotion, and Trust Metrics

A nurse enters a hospital room for a routine blood draw. She greets the patient, explains why she is there, and begins the task. Once finished, she asks if there is anything else she can do and swiftly exits. From the provider’s perspective, the interaction is efficient and smooth.
For the patient, however, it is a different experience. This is a moment of stress. His mind races with thoughts of bad outcomes. His blood pressure rises and his muscles tense as he anticipates the needle. What takes the nurse less than five minutes feels much longer. Even though the procedure goes well, he’s already anxious about the next visit.
One small shift could have made a world of difference: treating the patient as more than a task. A brief pause to acknowledge the person behind the procedure. A reassuring smile, a calming word, or even a simple, “Take a deep breath; we’ll get through this together.” Each a small but powerful gesture to ease the patient’s fear and transform the interaction into one of care and connection.
This is patient experience.
Once perceived as a healthcare “nicety” compared to service satisfaction scores, patient experience (PX) management now is a must-have when it comes to maximizing healthcare performance and improving medical outcomes.
- Hospitals with higher patient experience scores report a 161% better net margin than competitors with low scores.[1]
- A good patient experience correlates to a lower medical malpractice risk. One study shows that every drop in PX scores on a five-point scale increases malpractice suits by 22%.[2]
- Improving the patient experience by focusing on more effective care generates greater employee satisfaction and less turnover.
- Patient experience influences provider loyalty. Research shows patients reporting poor-quality physician relationships are three times more likely to leave the practice.
- For disease prevention and management, patient experience generates better outcomes. Studies of diabetic and heart attack patients show greater self-management skills and improved quality of life when reporting positive interactions with providers.
- Effective communication from providers correlates to stronger adherence to medical advice and treatment plans, especially for patients with chronic conditions.
As the stakes of healthcare increase, the patient experience matters more than ever. The data clearly shows PX to be a true lifesaver—for patients and medical systems.
But how can healthcare providers deliver a consistently positive experience when every patient is different?
Four experience dimensions define the benchmarks that drive high-quality PX:
- Success
- Effort
- Emotion
- Trust
These elements work beyond traditional standardized satisfaction measurements to identify core issues impacting the patient experience and ways to improve them.
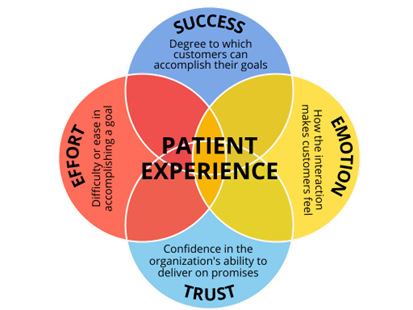
By using Success, Effort, Emotion, and Trust (SEET) as measurements for every PX process—from appointment setting to care plans to payments—the healthcare community can expand its potential for providing excellent care.
Beyond Surveys: A 360-Degree View of Patient Experience
No lack of metrics exists in healthcare, so why track four more things? The richness of the insights they provide.
Traditional tools like patient satisfaction surveys and Net Promoter Score (NPS) offer valuable performance snapshots but focus on isolated metrics. This limited scope can leave providers blind to deeper issues affecting care quality.
By contrast, Success, Effort, Emotion, and Trust work together to uncover the nuances of patient experiences. They don’t just measure outcomes but explore the emotional, functional, and relational factors driving them. Together with NPS and satisfaction assessments, these four drivers help healthcare organizations create a more comprehensive picture of patient needs, empowering them to prioritize and pursue improvements.
Measuring Quality Care: Patient Satisfaction Vs. Patient Experience
Patient satisfaction and patient experience measurements work in tandem to help medical providers deliver human-centered care. Institutions often use the terms interchangeably, but they represent distinct concepts.
Patient Satisfaction assesses how well an interaction or touchpoint meets a patient’s expectations for care. With consumerism at an all-time high in healthcare, people want to be treated like the valuable customers they are. When health systems meet expectations across the care continuum, they are more likely to increase loyalty and patient lifetime value.
Patient Experience focuses on how well encounters meet a patient’s perceptions of care. The Beryl Institute defines patient experience as the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care. This encompasses both major and minor interactions from provider communication to hospital stays and even parking availability.
Satisfaction compares what happened during an interaction to the customer’s expectations for what should occur. Experience is the interpretation of an interaction relative to the patient’s beliefs and the healthcare system’s standards for care. Satisfaction is more transactional, focusing on specific exchanges. Experience is relational, comprising the entire patient journey, range of emotions, and long-term connections. Together, they reveal critical insights for improving care quality.
Improving PX and the Problem with NPS
Many healthcare systems rely on NPS to evaluate patient experience. While NPS measures loyalty by asking if patients would recommend the organization, it provides limited insights into why patients feel the way they do.
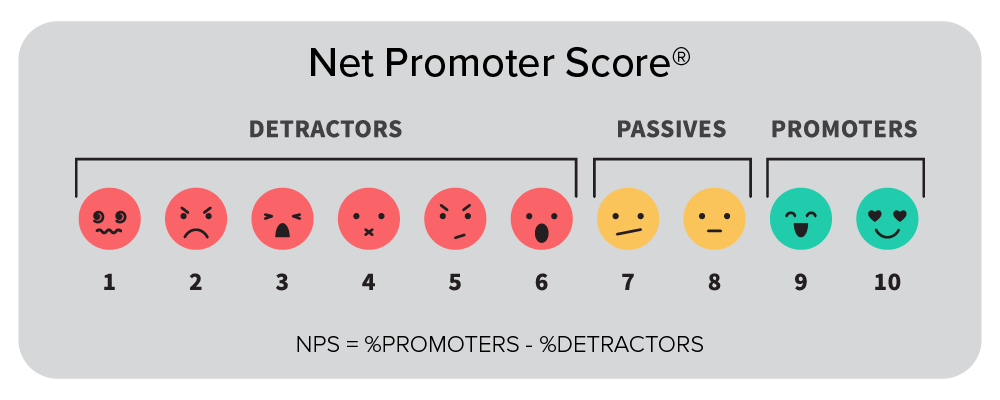
The four experience dimensions fill this gap by analyzing the functionality, accessibility, and responsiveness of the patient experience. These insights enhance understanding of:
- The way patients perceive their care
- How patients feel about the organization
- Patient loyalty and word-of-mouth recommendations
By layering in Success, Effort, Emotion, and Trust with NPS and satisfaction metrics, healthcare organizations can move beyond static scores to identify meaningful opportunities for systemic improvement. This holistic approach creates happier, healthier patients and a more resilient system.
Understanding the Four Components of PX
The four experience drivers account for what the patient journey should look like and offer data on how to make enhancements. When organizations score well across the four dimensions, they demonstrate their ability to meet patient needs. These healthcare institutions benefit from longer relationships (sometimes spanning generations), better patient outcomes, and increased community trust. It is a win for everyone.
The Four Drivers of Patient Experience
| Success (Functionality) | Effort (Accessibility) | Emotion (Responsiveness) | Trust (Confidence) |
| Goal attainment is the main point of the interaction and fundamental to receiving quality care. Success includes meeting patient needs at every touchpoint. | Effort impacts human behavior and healthcare compliance. Patients will end the journey if achieving success is complicated. | Feelings influence healthcare decision-making and patient outcomes. Minimizing negative emotions correlates to higher success and trust. | Organizations earn trust by keeping promises over time to develop credibility. Greater levels of trust contribute to improved care and patient loyalty. |
| Did you accomplish your goal? How successful were you in getting the care you needed? | How easy or difficult was it to accomplish your goal? How much energy did it take to get the care you needed? | How did the experience make you feel? How well did you feel cared for? | How much do you trust this facility and/or staff? How much faith do you have in our ability to deliver the quality care you need? |
Putting the Four PX Dimensions to Work
Elevating PX takes time and a willingness to see things through the eyes of the patient. The following steps outline how healthcare providers can implement the four key PX dimensions. The process turns valuable data into actionable insights that lead to long-term improvements.
1. Understand the patient population’s needs
Key to developing a quality patient experience is understanding what individuals, including their caregivers, require from the care journey. The process includes considering factors such as patient preferences, personal values, and demographic data. Providers should account for how people need to access their healthcare. Soliciting feedback from underrepresented voices within the patient population is important.
The goal is clearly defining what patients want, the services they need, and a standard of care that aligns with both. This level of understanding helps healthcare providers identify gaps that exist between what the system provides and what the patient needs to feel cared for and supported.
2. Map the patient journey
Journey mapping creates a visual representation of every interaction each patient persona has across the care continuum. No touchpoint is too small for inclusion. In addition to direct encounters with doctors and nurses, document additional aspects of the journey like searching for a provider, setting appointments, navigating a healthcare campus, accessing follow-up records, paying a bill, or getting a prescription. The journey map should include every step in the care process from A to Z.
Patient journey mapping shows exactly how people interact with a healthcare system. The process breaks down complex journeys spanning multiple touchpoints to create a better understanding of what patients and providers go through. The exercise is helpful for identifying unmet needs, current pain points, and differences between the intended and actual experience.
3. Collect data and generate insights
With the journey map complete, consider what Success, Effort, Emotion, and Trust should look like for every interaction. Now collect the data to establish benchmarks through the following:
- Conversation analysis
- Patient and provider surveys
- Focus groups
- Personal interviews
- Social listening
- Online review and rating studies
Using a combination of methods provides a more comprehensive understanding of the patient experience. The data helps identify improvement areas, compare experiences, and set quality care standards.
4. Share the findings with care providers
Everyone, from the custodial staff to the c-suite, impact the patient experience. Share data insights across the healthcare system. Focus the information on what each group can help control. Tie the data to systemic goals to improve buy-in.
By understanding patient perspectives and current performance, the system can collectively work toward continuous improvements that create a higher quality of care. Data also helps promote accountability toward performance goals. When healthcare institutions align around patient-centered care from top to bottom, the entire organization performs better financially and medically. Patient outcomes improve as well.
PX Improvements in Action: Serving Limited-English Patients
According to the American Medical Association, patients with limited English proficiency (LEP) experience higher rates of medical errors, worse clinical outcomes, and lower quality care. To better serve this vulnerable population, one healthcare system created a journey map specifically for LEP patients to find where they required additional language support.
The exercise identified four key touchpoints:
- During pre-op to understand the procedure
- At hospital admission when signing forms
- Immediately before surgery to ease anxiety and conduct the preoperative assessment
- In recovery to discuss how the procedure went and discharge instructions
The LEP journey map was the catalyst for systemic improvements that generated two significant outcomes. First, by instituting a language plan, LEP patients became less likely to experience issues during their care. The healthcare provider also generated cost savings by investing where patients needed language services most rather than relying solely on expensive on-demand translation services.
5. Set improvement priorities and take action
The data will unearth plenty of opportunities for improvement. One of the biggest mistakes organizations make is trying to “boil the ocean” by resolving too many things at once. This almost always results in PX initiative failures and delays.
Narrow the areas that need attention to the most important. Identify who should be involved and the resources required. Establish timelines for implementing changes. Share the priorities and make them easily accessible. They should be front and center to maintain a long-term focus rather than feeling like another improvement fad.
Start small and think long-term.
- Select minor fixes that can generate major wins. Consistent, incremental changes help create buy-in with staff and trust among patients. They create momentum. Celebrate each success to keep the progress going.
- Develop a PX improvement road map. Work from a multi-year plan that outlines what needs to change, the actions required, and the intended outcomes. Establish timelines for each improvement initiative.
- Monitor the four PX dimensions and refine the plan. Measure performance against the Success, Effort, Emotion, and Trust benchmarks established in the data collection process. Track how improvements are impacting the metrics and adjust accordingly.
PX Improvements in Action: Promoting Patient Autonomy
A healthcare system found that patients wanted greater autonomy while hospitalized. The medical facility implemented on-demand service buttons to request things like blankets or meal removals. By streamlining basic requests, the hospital met a patient demand while also limiting the need to involve busy nurses. The small change improved patient satisfaction and decreased errors caused by non-medical nursing interruptions.
A SEET at the Table
Healthcare systems incorporating the four key drivers of PX—Success, Effort, Emotion, and Trust—give patients a “SEET” at the table by putting them at the center of every care interaction. Each touchpoint becomes a valuable opportunity to develop a trusted relationship. These core dimensions ensure patients feel heard, valued, and understood. This is the essence of elevating healthcare quality.
[1] Value of Patient Experience. Deloitte United States. https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/hospitals-patient-experience.html
[2] Why Improve Patient Experience? Agency for Healthcare Research and Quality. https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/2-why-improve/index.html.